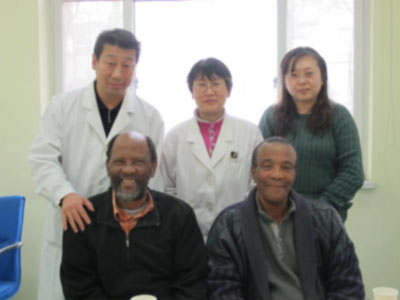
Rampe - ALS (South Africa) Posted on January 20, 2014
Name:Rampe Daniel Phetoe 
Sex:Male
Age:67 years old
Country: South Africa
Diagnoses: 1.Amyotrophic lateral sclerosis 2.Type 2 diabetes
Admission Date: 2013-11-30
Days Admitted to the Hospital:28
Before treatment:
The patient suffered from numbness and weakness of his right lower limb 2 years ago without obvious inducement. He was diagnosed with diabetes by a doctor and received hypoglycemic agent for treatment, but the condition did not improve. His muscles then atrophied and the weakness of right lower limb was aggravated gradually. He needed support to walk, therefore, was using walking stick to aid him walk. About a year later, the patient's left lower limb had the same condition. This resulted in inability of the patient to walk. So he went to a local hospital for therapy and received EMG examination. The motor neuron disease was considered. He didn't receive medication for treatment. The patient suffered from weakness and muscle atrophy of his right shoulder. He was unable to take care of himself completely. From the onset of disease, the patient had normal urination and defecation. His mood was stable. The diet and sleep were normal. He had no dizziness or headache. The patient’s mother had diabetes. There was no other genetic disease.
Admission PE:
Bp: 133/88mmHg; Hr: 72/min, temperature 36.3 deg. Br: 18/min. The nutrition was normal. The body type was normal. His skin and mucosa was normal, with no yellow stains or petechia. The respiratory sounds in both lungs were clear, with no obvious rales. The heart sounds were low and blunt. The rhythm of his heartbeat was normal with no obvious murmur in the valves. His abdomen was enlarged and soft, with no pressing pain or rebound tenderness in the abdomen. The doctor did not touch the liver or spleen under the ribs. There was mild pitting edema in both ankles and dorsal.
Nervous System Examination:
Rampe Daniel Phetoe was alert and his sprit was good. His memory, calculation abilities and orientation were all normal. Both pupils were equal in size, the diameter was 3mms. Both eyeballs could move flexibly and the pupils reacted normally to light stimulus. Both eyeballs had slight horizontal nystagmus. The convergence ability of both eyeballs was normal. The forehead wrinkle pattern was symmetrical. He was able to close his eyes with ease. The bilateral nasolabial sulcus was equal in depth. The corners of mouth were symmetry and the tongue was at the center of the oral cavity. There was no obvious atrophy of the tongue. The tongue could move freely. He had strong strength to raise his soft palate. The uvula was at the center of oral cavity. The neck was soft with strong muscle to turn his head left side and right side. His right side had slight weak muscle strength to shrug the shoulder. The left side had almost normal muscle strength to shrug the shoulder. The muscle strength of left upper limb's near end was at level 3+, and the far end was at level 4. The grasp power of left hand was at level 5-. The muscle strength of right upper limb's near end was at level 3, and the far end was at level 4-. The grasp power of right hand was at level 4+. The muscle strength of both lower limbs was at level 0. The muscle tone of his four limbs was almost normal. The tendon reflex of his four limbs disappeared. There was muscle atrophy in both metacarpophalangeal and interphalangeal joints and the bilateral supraspinatus. There was also obvious muscle atrophy in bilateral biceps femoris muscle, quadriceps femoris and gastrocnemius muscle. Bilateral abdominal reflex was not elicited. Bilateral jaw reflex and palm jaw reflex were negative. The sucking reflex was negative. The Hoffmann sign was negative. Bilateral Babinski sign was not elicited. The deep sensation and shallow sensation, using loose measures, were normal. He was able to finish the finger-to-nose test, the digit opposition test and rapid rotation test in a stable manner. He was unable to finish the heel-knee-shin test. The meningeal irritation sign was negative. The assisted examination: EMG (2012.6.25) : Early spinal cord anterior horn cells disease.
Treatment:
The patient received treatment from November 30, 2013. The patient received nerve regeneration treatment and stem cell activating treatment. At the same time, he received treatment to improve his blood circulation in order to increase the blood supply to the damaged neurons, to repair the damaged neurons and to nourish them. He also received treatment to protect his organ and also to control his blood sugar. This was accompanied by daily physical rehabilitation training.
Post treatment:
The patient's exercise tolerance has improved obviously. The muscle strength of both lower limbs has increased than before. The muscle strength of both lower limbs' near-end has reached level 2 and the far-end at level 2. With some assistance, the patient can stand and raise both legs and can lift legs in bed. The blood sugar is under control. The blood glucose is almost stable and under control. The blood sugar measured 2 hours after the meal or an empty stomach is in the normal range.
Email:
Date: Mon, Nov 17, 2014
Dear Mary
I placed an order for Daniel Medication, I just want to check how far are you with his order, the following is what he need:
1. Flunarizin
2. Folic Acid
3. Oryzamol
4. Multivitamin
Please advice on his medical report that I Have send it to you on the 10 October 2014.
Regards
Pholoso
