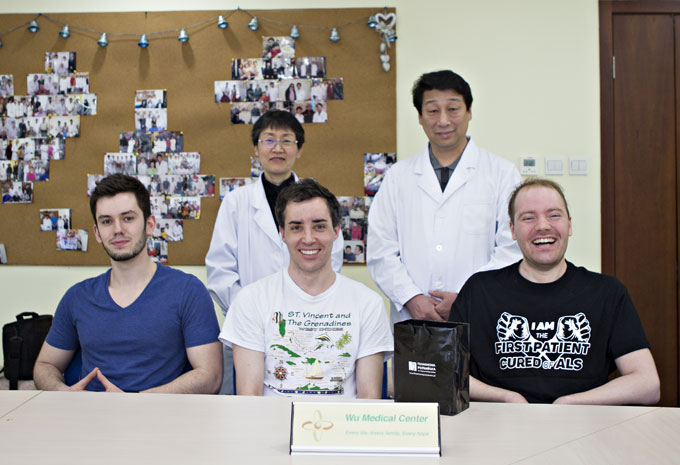
Michal Luczak-Amyotrophic Lateral Sclerosis-(Poland)-Update on March.30th, 2017
 The second round of treatment:
The second round of treatment:
Name: Michal Luczak
Sex: Male
Nationality: Polish
Age: 29Y
Diagnosis: Amyotrophic lateral sclerosis
Date of Admission: November 6th, 2016
Treatment hospital/period: Wu Medical Center/12days
Before treatment:
Michal felt weakness in his right hand and didn’t know what the cause was. This was in May 2014 and five months later his right leg became weak. When he walked, he was not able to raise his right leg but the sensations in the leg were normal. He went to the local hospital and had an MRI, EMG and genetic tests performed. He was diagnosed with amyotrophic lateral sclerosis (ALS) in November 2014. He was prescribed Riluzole but the symptoms still got worse. All four limbs were weak, along with muscular atrophy and muscular tremors. He was not able to speak clearly, his breathing was fast and shallow, and he would often choke when he drank. He came to our hospital 6 months ago. After treatment his upper limbs were powerful and his breathing and swallowing function were improved. He received lumbar surgery 4 months ago but his muscle power became worse, his muscle tone was weaker and he was unable to move well. At present, he is unable to sit up, turn over, stand or take care of himself. He wants a better life so he came to our hospital again and was diagnosed with Amyotrophic lateral sclerosis.
His mental health, diet, bladder and bowel action are all good, but his sleep pattern is bad and he has lost 16 kg.
Admission PE:
Bp: 114/74mmHg, Hr: 74/min, breathing rate: 20/min, body temperature: 36 degrees. Nutrition status is normal and he has normal physical development. There is no injury or bleeding spots of his skin and mucosa, no blausucht, no throat congestion, and his tonsils have not swollen. Chest development is normal but his chest movement is weaker than normal. The respiratory sounds in both lungs were clear but the breathing sound of the lower lungs is slightly weaker but there were no dry or moist rales. The heart beat is powerful with regular cardiac rhythm and with no obvious murmur in the valves. The abdomen was soft and pliable, with no masses or tenderness. His liver and spleen were normal and there is no edema in both lower limbs.
Nervous System Examination:
The patient was alert but has slurred speech. His memory, orientation and calculation ability were normal. Both pupils were equal in size and round, with a diameter of 3mm, they react well to light and the eyeballs can move freely. There is no nystagmus. Bilateral forehead wrinkle and nasolabial fold are symmetrical and he can close his eyes strongly. His tongue is in middle with tongue muscle atrophy but he can only can extend his tongue out to the lips on the sides. Tongue movement ability is poor. His tongue can not touch the cheeks powerfully. Showing teeth is normal, but the patient cannot bulge his cheeks out strongly. His chewing ability is weaker than normal. Bilateral soft palate can lift as normal, pharyngeal reflex is normal but his swallowing function is bad, the mouth bulges when drinking. There is obvious muscle atrophy of the sternocleidomastoid muscle, shoulder girdle muscles, bilateral forearms muscles, hands interosseous muscles, thenar muscles, and lower limbs muscles.
He can;
Turn his neck with muscle power of 4 degrees, shoulder shrug muscle power is 1 degree, the left arm flexor muscle power is 3- degrees, extensor muscle power is 3+ degrees, grip force of left hand is 2- degrees, the right arm flexor muscle power is 2+ degrees, extensor muscle power is 3- degrees, right hand grip force is 1 degree. Muscle power of lower limbs is 2+ degrees.
Muscle tone of the 4 limbs is higher than normal and he has muscle spasm when he move his arms and legs. The patient had hyperreflexia of the bilateral Biceps tendon reflex and abdominal reflex can not be induced by examination. Bilateral Hoffmann and Babinski signs are positive. His deep and superficial sensations are normal by full examination. He can not perform the finger opposite test, fast alternative test and finger to nose test. The patient can not do the heel-knee-tibia test himself. Meningeal irritation sign is negative.
Treatment:
After the admission, he was diagnosed with ALS. He received 3 neural stem cell injections and 3 mesenchymal stem cell injections to repair his damaged motor nerves and we replaced dead nerves with new injected stem cells. We nourished nerves and improved blood circulation, improved the immune system function and doctors gave the patient a BI-PAP breathing machine to assist his breathing function. The parameters are: S/T model, IPAP 15cm H2O; EPAP 6cm H2O, breathing rate as 14/min. The patient also received treatment for his speech and swallowing function with training and rehabilitation.
Post-treatment:
After 12 days of treatment the patient can now extend his tongue out of the lips a little more. His tongue muscle movement ability is more flexible and muscle spasm of the upper limbs is reduced. The grip strength of both hands increased with the grip strength of the left hand level 3-, and grip strength of right hand level 2. Muscle power of distal lower limbs is 3+ degrees, proximal side is 3- degrees. Both his energy and spirits are improved.




The first round of treatment:
Date of Admission: Mar.27, 2016
Treatment hospital/period: Wu Medical Center/17 days
Before treatment:
Michal felt weakness in his right hand and didn’t know what the cause was, in May 2014, and five months later, his right leg became weak. When he walked, he was not able to raise his right leg but the sensations in the leg were normal. He went to the local hospital and had an MRI, EMG and genetic test performed. He was diagnosed with amyotrophic lateral sclerosis (ALS) in November 2014. He was prescribed Riluzole but the symptoms still got worse. All four limbs were weak, along with muscular atrophy and muscular tremors. He was not able to speak clearly 5 months ago, his breathing was fast and shallow, and he would often choke when he drank. It is difficult for him to walk right now, he is only able to walk slowly with assistance, and he is not able to sit up, turn over or stand up by himself. He is not able to dress himself, wash his face or eat food unassisted. He constantly requires someone to care for him. Michal was diagnosed with ALS when he first arrived at our hospital.
Michal has lost 16kg since the onset of the disease. He’s in good spirits. His diet is normal. He is not getting enough sleep.
Admission PE:
Bp: 136/92mmHg; Hr: 92/min. Br: 20/min. Temperature: 36.5 degrees. Sat:94%. There were no yellow stains or petechia on the skin or mucosa. There was no pharyngeal congestion. The tonsils were not enlarged. The thorax was symmetrical. The wave signals were weak. The respiration in the base of both lungs was weaker than normal. The respiration in the apex of both lungs was clear. There were no dry or moist rales. The rhythm of the heartbeat was normal with no obvious murmur in the valves. The abdomen was soft and flat with no pressing pain or rebound tenderness. The liver and spleen were normal. There was no edema in the lower limbs. There was obvious muscular atrophy in the sternocleidomastoid, shoulder girdle, forearms, interosseus of both hands, thenar, hypothenar and both lower limbs.
Nervous System Examination:
Michal Luczak was alert and in good spirits. He was not able to speak clearly. His memory, calculation ability and orientation were normal. Both pupils were equal in size and round, the diameter was 3mms.Both eyes had sensitive responses to light stimuli. Both eyeballs could move freely. The nasolabial fold and forehead wrinkle pattern was symmetrical. Michal could close his eyes strongly. The tongue was centered in the oral cavity. The movement of the tongue was basically normal but he was not able to touch the inside of the cheeks. The tongue muscle was not atrophied but there were tongue muscle ventricular fibrillations. The teeth were not deflected. There was some leakage of air when the cheeks were expanded. He was not able to chew well. Both soft palates could be raised, and the pharyngeal reflex was normal, but there was difficulty with swallowing. Michal would often choke when drinking liquids as a result. The neck muscles were powerful, and the turning power of the head was at level 5. The muscle power of the shoulders was at level 1. Left side: The abduction muscle power of the left upper limb was at level 2, the flexor muscle power was at level 4-, the extensor muscle power was at level 4-. The muscle power of the wrist flexion and extension was at level 1, the left hand grip was at level 2. Right side: The abduction muscle power of the right upper limb was at level 2, the flexor muscle power was at level 4-, the extensor muscle power was at level 3. The muscle power of the wrist flexion and extension was at level 1, the right hand grip was at level 1. The muscle power of the lower limbs was at level 3-. The muscle tension of all four limbs was a little higher, especially the lower limbs. The bilateral biceps brachii reflex, radial periosteal reflex, triceps brachii reflex, patella tendon reflex and achilles reflex were over active, the abdominal reflex was normal. The bilateral wrist clonus, palm jaw reflex, sucking reflex, Hoffmann’s sign, Rossolimo’s sign and Babinski’s sign were positive. The deep sensation and superficial sensation on both sides were normal. Michal was able to do the finger-to-nose test and rapid rotation test slowly. He was not able to do the heel-knee-tibia test or the finger–to-nose test. The meningeal irritation sign was negative.
Treatment:
Michal was diagnosed with amyotrophic lateral sclerosis (ALS). He received four neural stem cell injections and four mesenchymal stem cell injections to repair his damaged nerves, regenerate new and normal nerves, activate the stem cells in his body, nourish the neurons, and regulate his immune system. He also had daily physical rehabilitation training.
Post-treatment:
After 17 days of treatment, Michal had better pronunciation, he was able to chew powerfully, and his swallowing ability was better. He was able to hiccup. His physical endurance was improved, and he was able to breathe better. The sat was raised from 94% to 97%. The gripping strength of his right hand was at level 4, the left hand was at level 3. The abducent muscle power and wrist flexion muscle power in the left upper limb were both at level 3. He had lower muscle tension.




E-mails:
Date:2016-8-1