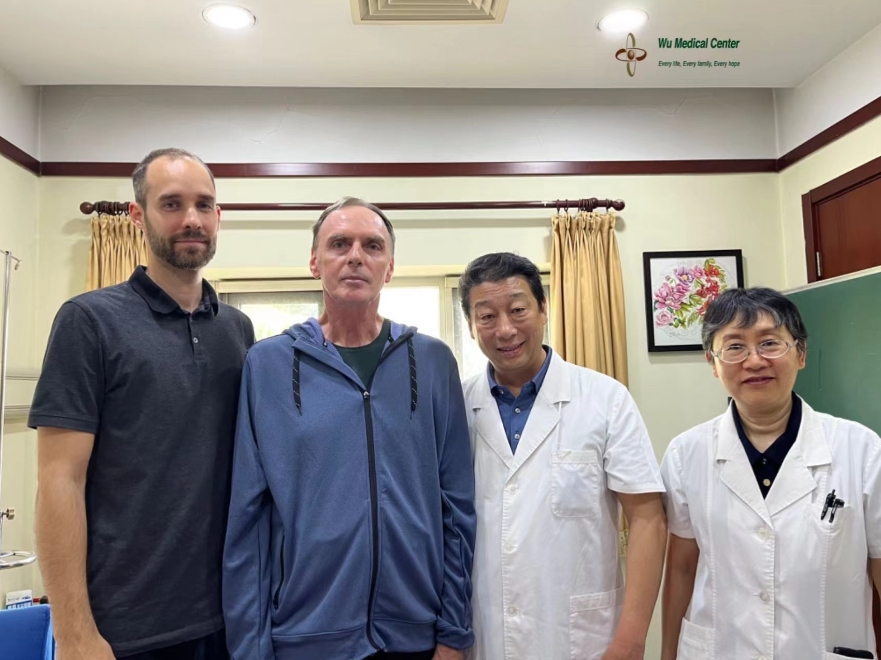
Pálfalvai Zoltán-Amyotrophic lateral sclerosis (ALS)-(Hungarian)
 Patient's name: Pálfalvai Zoltán
Patient's name: Pálfalvai Zoltán
Gender: Male
Age: 61 years old
Nationality: Hungarian
Diagnosis: Amyotrophic lateral sclerosis (ALS)
On admission:
The patient developed weakness of the right upper limb two years ago (March 22, 2022). He was diagnosed with "amyotrophic lateral sclerosis" at a local hospital and has been taking riluzole and tauroursodeoxycholic acid for treatment, but the effect was not obvious and the disease was still progressing. He had mitral valve prolapse (the specific time is unknown) and did not take any related medication. Currently, his all four limbs have decreased muscle strength, with the right upper limb being the most severe. His right upper limb strength has almost completely declined, and he could slowly lift his left hand up to his jaw. His voice was somewhat slurred; there was no noticeable difficulty swallowing or drinking choking.
Admission physical examination:
The patient's pulse was 64 beats/min, his respiratory rate was 18 breaths/min, his blood pressure was 131/84 mmHg, and his oxygen saturation was 91%. He was of normal development, with average nutrition and a thin build. His lips and tongue were without cyanosis, and there was no redness or swelling in his pharynx. His thorax was symmetrical, with slightly weak respiratory movement, and clear breath sounds were heard in his both lower lungs, without obvious dry or moist rales. His heartbeat was strong and regular, and there was a strong, regular heart murmur during systole. His abdomen was flat and soft, with the liver and spleen not palpable. There was no edema in both lower limbs.
Neurological Examination:
The patient was alert and had a normal mental state. His speech was slightly unclear. His memory, calculation ability, and orientation were all normal. His pupils were 3mm in diameter and respond to light stimuli with sensitivity. His eyes had flexible movements in all directions. The symmetry of his nasolabial folds and forehead wrinkles was normal, and his tongue was extended centrally. His tongue muscle was atrophic, with mild weakness in tongue movement. His cheek muscle strength was normal, his chewing ability was normal and there was no water swallowing choking. His bilateral soft palate lift was also normal, and the uvula was centered. He had neck rotation and scapular shrug with muscle strength grade 4, and his left proximal upper limb was slightly weaker with muscle strength grade 2+, which could lift to his jaw slightly when lying down. His right upper limb had muscle strength grade 1+ but was difficult to move and only showed muscle contraction when lying down. His lower limbs had muscle strength grade 4 with walking drag, allowing him to walk on his own with a noticeable decrease in gait speed and increased fatigue. Muscle atrophy was present in his all four limbs, accompanied by muscle twitching. His limbs had normal sensation and normal muscle tone, with active tendon reflexes in his all four limbs. The Babinski sign was positive in his both lower limbs. His left hand finger-nose test was extremely poor, and his right hand could not complete it due to muscle strength reasons. In the index testing, he could do it for thumb and index finger on his left hand, but could not do it for the rest of his fingers, while his right hand could not complete the test due to muscle strength reasons. On his both hands, during the hands-in-rotation test, his left hand performance was poor, his right hand could not complete the test due to muscle strength reasons. He also had unsatisfactory performance in the heel-knee-shin test on both legs. His cerebrospinal meningitis sign was negative.
Treatment process:
The patient was admitted with a clear diagnosis of "amyotrophic lateral sclerosis" (ALS). During his hospital stay, he received neural stem cell therapy to repair motor nerve damage, mesenchymal stem cell therapy for nutritional, endocrine, and immune support, and adjuvant medication including edaravone, riluzole, and nerve growth factor. Additionally, he received comprehensive rehabilitation treatment.
Post-treatment:
The patient's motor function has significantly improved. His muscle strength has increased, with his left upper extremity proximal muscle strength improving to grade 3+. He can raise his left arm straight and maintain it for up to 10 seconds when supine. His left hand grip strength is grade 3+, allowing him to grasp and hold onto others' fingers with some resistance. His right upper extremity muscle strength is grade 2+, and his right arm can be moved freely on the bed surface and undergo internal rotation. Some fingers of his right hand can be bent. The muscle volume of both arms has increased compared to his admission status. His left hand's ability to perform the index test is essentially complete, and his hand-in-rotation test performance has improved. His heel-knee-shin test performance has also improved. His abdominal and back muscle strength has increased, his movement speed has improved, and his flexibility has increased. His blood oxygen saturation has improved, and he can achieve a saturation of 94% without a ventilator. His energy, physical stamina, and exercise endurance have all improved.